16 May Interview Julio Mayol – Professor of Surgery at the Complutense University of Madrid and Head of the Colorectal Surgery Section at the Hospital Clínico San Carlos
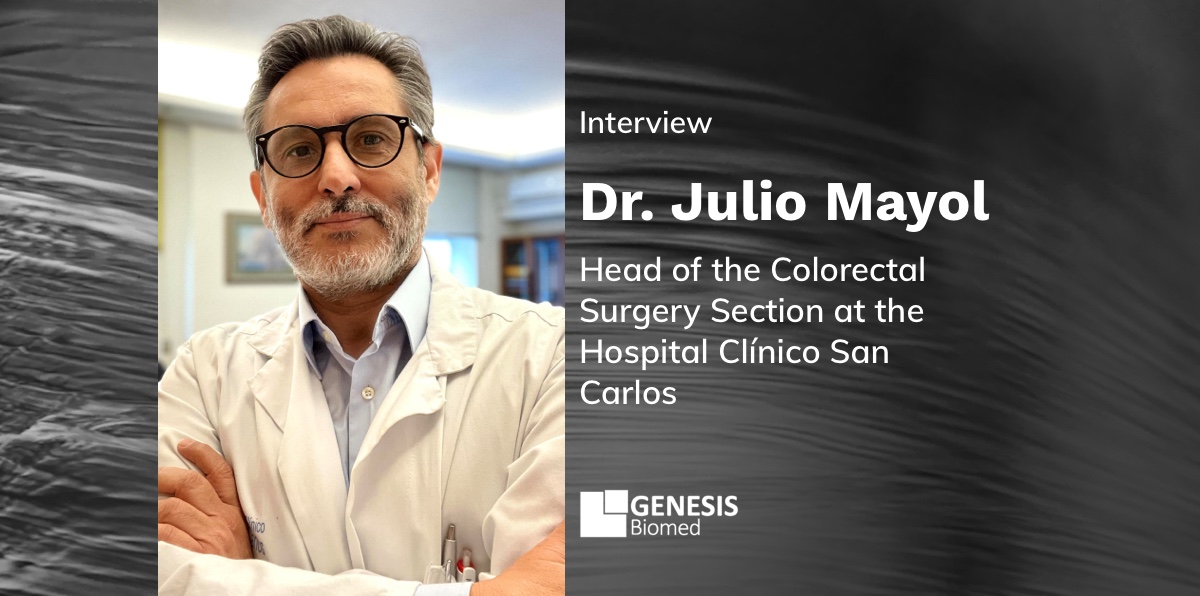
Julio Mayol: “In order to advance the National Health System Digital Health Record (NHSDHR), a shared vision is needed in terms of integration and interoperability, which facilitates closer collaboration between health authorities at regional and national level”.
Professor of Surgery at the Complutense University of Madrid and Head of the Colorectal Surgery Section at the Hospital Clínico San Carlos, where he held the position of Medical Director between 2016 and 2023. Delegate of the Dean of the Faculty of Medicine UCM for new technologies and communication. Director of the Innovation, Surgery, Pharmacy and Neuroengineering Group of the San Carlos Institute for Health Research (IdSSC), trustee of the San Carlos Biomedical Research Foundation, where he also serves as Vice-President.
He is secretary of the BJS Society (formerly known as the British Journal of Surgery), and a member of its board of editors and editor of the US journal Surgery. In addition, he also acts as editorial advisor to other relevant journals in the field of surgery and gastroenterology (Journal of Gastrointestinal Surgery, World Journal of Gastroenterology, Turkish Journal of Surgery and European Journal of Anatomy).
Is the National Health System Digital Health Record (NHSDHR) with information from each patient’s Health Record a reality or are there still problems of integration and interoperability between data from different Autonomous Regions?
Although few professionals make use of the solutions that allow access to the NHSDHR, progress has undoubtedly been made in its implementation. Even so, significant challenges remain in terms of integration and interoperability between data from different autonomous communities, at the technological, semantic and organisational levels. This is due to multiple reasons including differences in health information systems, organisational culture, the existence of heterogeneous data protocols and a lack of standardisation in the capture and exchange of information. Asymmetries in the availability of technological resources and data privacy and governance policies have also contributed to fragmentation into silos of information that are almost impossible to break down. To address these problems, a shared vision is needed to facilitate closer collaboration between health authorities at regional and national levels, as well as the adoption of more robust interoperability standards and investment in adequate technological infrastructure.
After the pandemic, the use of private health insurance has continued to grow. Do you think there should be an initiative to incorporate all this data into the NHSDHR?
The increase in private health insurance after the pandemic presents, as always, an opportunity and a challenge for the integration of data into the health system. In addition to the people who take out private insurance, it should be noted that almost 3 million citizens (civil servants of the state administration) belong to the mutual insurance system, whose services (and consequently data) are in the private system.
Incorporating this data into the NHSDHR could provide a more complete picture, which in turn would facilitate better coordination between the public and private sector.
Proposals for solutions have been launched from the private sector. However, this poses challenges related to data security and privacy, as well as to the standardisation of data formats used by private insurers. Clear policies and robust security measures would be needed to guarantee the confidentiality of patient data and promote collaboration between the different actors in the health system.
In a recent agreement, the European Health Data Space (EHDS) has been launched. Do you think we are lagging behind in European or national regulatory frameworks that allow for an enabling framework for sharing secondary use of health data?
The launch of the European Health Data Space is an important step towards the integration of health data at European level. However, there are gaps in both European and national regulatory frameworks that hinder the secure and efficient exchange of health information for research and clinical care purposes. Barriers include concerns about privacy and data security, as well as the lack of common standards for interoperability between health information systems.
Spain has been one of the countries that has most strongly promoted the EHDS during its presidency of the EU. However, the very model of financing and operation of the Bismark systems (Germany, France, with private providers) has caused resistance to change and doubts about the desirability and feasibility of the system. To overcome these obstacles, further harmonisation of data protection laws across Europe is required, as well as the promotion of interoperable technical standards and the promotion of transparent and ethical data governance practices.
There is great fear among patients that their health data will be used, even though it is pseudo-anonymised and the GDPR provides a solid basis for its use. Do you think there is a lack of public awareness of the need for the use of such data in research?
Patients’ fear of their health data being used, even when pseudo-anonymised, reflects legitimate concerns about the privacy and security of health information. Although the GDPR provides a robust legal framework for the use of data in research, misunderstandings and mistrust persist among the general public about how their health data are used and protected.
Addressing this problem requires greater education and awareness of the benefits of data-driven research to improve care and develop new treatments. In addition, it is crucial to establish clear mechanisms for informed consent (or informed request by patients) and privacy safeguards to ensure that patients have control over the use of their data and that their rights are respected.
How do you think the secondary use of health data and the use of AI will impact 5P (predictive, preventive, participatory, personalised and population-based) medicine and specifically Personalised Medicine?
The secondary use of health data and the application of artificial intelligence in 5P (predictive, preventive, participatory, personalised and population-based) medicine have the potential to transform care by improving the value obtained from care interventions. However, it is critical to address important challenges related to data quality and integrity, interpretation of AI results, and equity and ethics in the use of health technologies. Interdisciplinary collaboration between clinicians, data scientists, other healthcare professionals, managers, regulators and society as a whole is needed to fully harness the transformative potential of these technological advances while mitigating risks and protecting patients’ rights.
In your opinion, to strengthen the sustainability of the system, should industry have access to health data generated in the public sector for use in its own biomedical research projects?
From my perspective, allowing industry access to public sector health data can be very beneficial for understanding system problems, planning actions and designing interventions, as long as there is a model of collaboration that ensures a meaningful and tangible return for the health system and for individuals, as well as reciprocity in the exchange of information.
The health data we generate in the public system, as well as belonging to patients, encapsulates an extensive clinical knowledge and professional expertise. If industry has access to this data, it should commit to sharing its own clinical trial data beyond reasonable time limits of use. This is not only fair, but it also enhances the global knowledge base and facilitates more rapid and informed advances in medicine.
The ethical model for data use must be symmetrical and congruent in its objectives to ensure that both the public sector and industry benefit mutually. Access should be managed in a way that promotes innovation and improves the quality of healthcare, without compromising patient privacy and data integrity.