13 Nov Chronic Inflammation: A Key Factor in the Threat to Healthy Aging and Healthy Living
Article by Natalia de la Figuera – Co-Founder and COO of GENESIS Biomed
• Chronic low-grade inflammation is emerging as a major driver of accelerated biological ageing.
• Recent research links persistent inflammatory status to metabolic, neurodegenerative and cardiovascular pathologies.
• Gut microbiota, diet and lifestyle are emerging as key factors in modulating inflammation and promoting healthy ageing.
• Prevention and personalisation, pillars of the new medical strategy against chronic inflammation
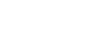
Ageing, traditionally understood as an inevitable biological process, has begun to be reconsidered from a new scientific perspective. It is now known that beyond the passage of time, the real enemy of healthy ageing is chronic low-grade inflammation, a silent state that progressively deteriorates tissues and accelerates the onset of age-related diseases.
Clinical and epidemiological studies have shown that this phenomenon, known as “inflammaging”, is central to the loss of cellular function and the development of diseases such as type 2 diabetes, Alzheimer’s, cardiovascular disease and certain cancers. In contrast to acute inflammation, a temporary, beneficial response of the immune system to infection or injury, chronic inflammation persists for years, causing constant wear and tear that disrupts the body’s homeostasis.
Chronic inflammation is closely associated with mitochondrial dysfunction, oxidative stress and altered epigenetic mechanisms. These alterations lead to an increase in pro-inflammatory cytokines (such as interleukin-6 or tumour necrosis factor-alpha), which act as chemical messengers of cell deterioration. Over time, this imbalance results in an accelerated biological ageing process, even in individuals who appear healthy. At the immune level, the ageing body loses the ability to adequately regulate its defence response. This phenomenon, called immunosenescence, weakens the response to infections and vaccines, while keeping inflammatory signals constantly active. The combination of both processes creates a vicious circle that progressively deteriorates organs and tissues.
To have a good quality of life as well as healthy ageing, it is important to reduce this chronic inflammation. Research on the gut microbiota has revolutionised the understanding of chronic inflammation. The microbial balance in the gut is known to regulate much of the immune system and modulate the production of inflammatory mediators. When this balance is disrupted (by poor diet, stress or excessive antibiotic use) dysbiosis occurs, a state that promotes intestinal permeability and the entry of toxins into the bloodstream, triggering systemic inflammatory responses. The gut-brain axis also comes into play in this context. Bidirectional communication between the digestive system and the central nervous system means that an altered microbiota can influence mood, sleep and general well-being, key elements of the healthy living concept. Modulation of the gut ecosystem through probiotics, prebiotics, postbiotics and synbiotics is one of the most promising strategies to combat chronic inflammation and improve quality of life in the elderly. Probiotics, live microorganisms that confer benefits to the host, help to restore microbial balance, strengthen the intestinal barrier and reduce the release of inflammatory mediators. In addition, psychobiotics, a new generation of probiotics and prebiotics with mental health effects, are showing potential in improving mood and reducing stress, factors that directly influence systemic inflammation. This holistic view, which integrates physical, digestive and emotional health, redefines the concept of healthy ageing under the premise that “taking care of the microbiota is taking care of the future of the organism”.
Caring for the microbiota also involves adopting healthy lifestyle habits that have been shown to reduce inflammatory cytokines and play a decisive role in controlling the inflammatory state. These healthy habits include.
- Diet: A Mediterranean diet, rich in fruits, vegetables, legumes, olive oil and oily fish contains fibre, polyphenols and fermented foods that not only improve digestion, but actively contributes to reducing chronic inflammation. In contrast, excessive intake of refined sugars, saturated fats and ultra-processed foods increases systemic inflammation.
- Regular physical exercise: This acts as a potent immunometabolic modulator. Studies have shown that moderate-intensity physical activity reduces the concentration of pro-inflammatory cytokines and improves mitochondrial function, promoting slower cellular ageing. In contrast, a sedentary lifestyle and obesity promote an inflammatory metabolic environment, increasing the risk of chronic diseases.
Addressing chronic inflammation as a central factor in ageing opens the door to preventive and personalised medicine. The therapeutic strategies of the future are geared towards identifying individual inflammatory biomarkers, studying specific microbial profiles and personalising diets and treatments according to each person’s immune response.
This new paradigm places the individual at the centre of the ageing process, promoting a lifestyle based on scientific evidence and self-management of health. The collaboration between medicine, nutrition, biotechnology and healthy habits is emerging as the most effective way to prolong functional longevity and preserve physical and mental well-being.